
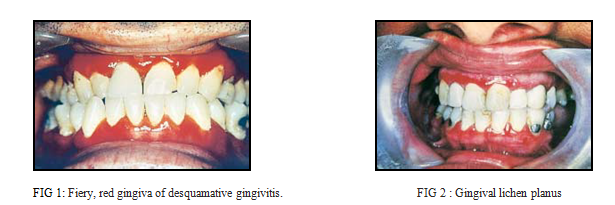
Desquamative gingivitis (DG) is a clinical description of the gingiva which may manifest as a result of various mucocutaneous conditions such as lichen planus or vesiculobullous disorders . It is characterized by fiery red, glazed, atrophic or eroded looking gingiva. There is loss of stippling and the gingiva may desquamate easily with minimal trauma (Fig 1, 2).
As opposed to plaque induced gingivitis, desquamative gingivitis is more common in middle-aged to elderly females, is painful, affects the buccal/labial gingiva predominantly, frequently spares the marginal gingiva but can involve the whole thickness of the attached gingiva and its clinical appearance is not significantly altered by traditional oral hygiene measures or conventional periodontal therapy alone.
The majority of cases of DG are now known to be due to mucocutaneous conditions, in particular lichen planus, pemphigoid and pemphigus. Other causes include allergic reactions to toothpastes/mouth rinses (plasma cell gingivitis), Crohn’s disease, psoriasis, linear IgA disease and chronic ulcerative stomatitis.Desquamative gingivitis can be mistaken for plaque induced gingivitis and this can lead to delayed diagnosis and inappropriate treatment of serious dermatological diseases such as pemphigoid or pemphigus.
Correct identification of these conditions entails taking a careful history and performing a thorough intra-oral examination. Presence of cutaneous, nasal, ocular and genital lesions should be carefully elicited from the patient. A definitive diagnosis depends on taking an incisional biopsy from a perilesional site (with intact epithelium) and sending a fresh specimen for immunostaining. If a blistering condition is diagnosed, referral to an appropriate specialist is advised. The gingival lesions are usually treated by improved oral hygiene measures and occlusive topical corticosteroid therapy.
For more info,visit: https://www.santosh.ac.in/

